Guidelines for Osteoporosis in the Elderly
Crack the code on osteoporosis in the elderly with essential guidelines for prevention, diagnosis, and treatment. Expert advice for healthy aging.
Understanding Osteoporosis in the Elderly
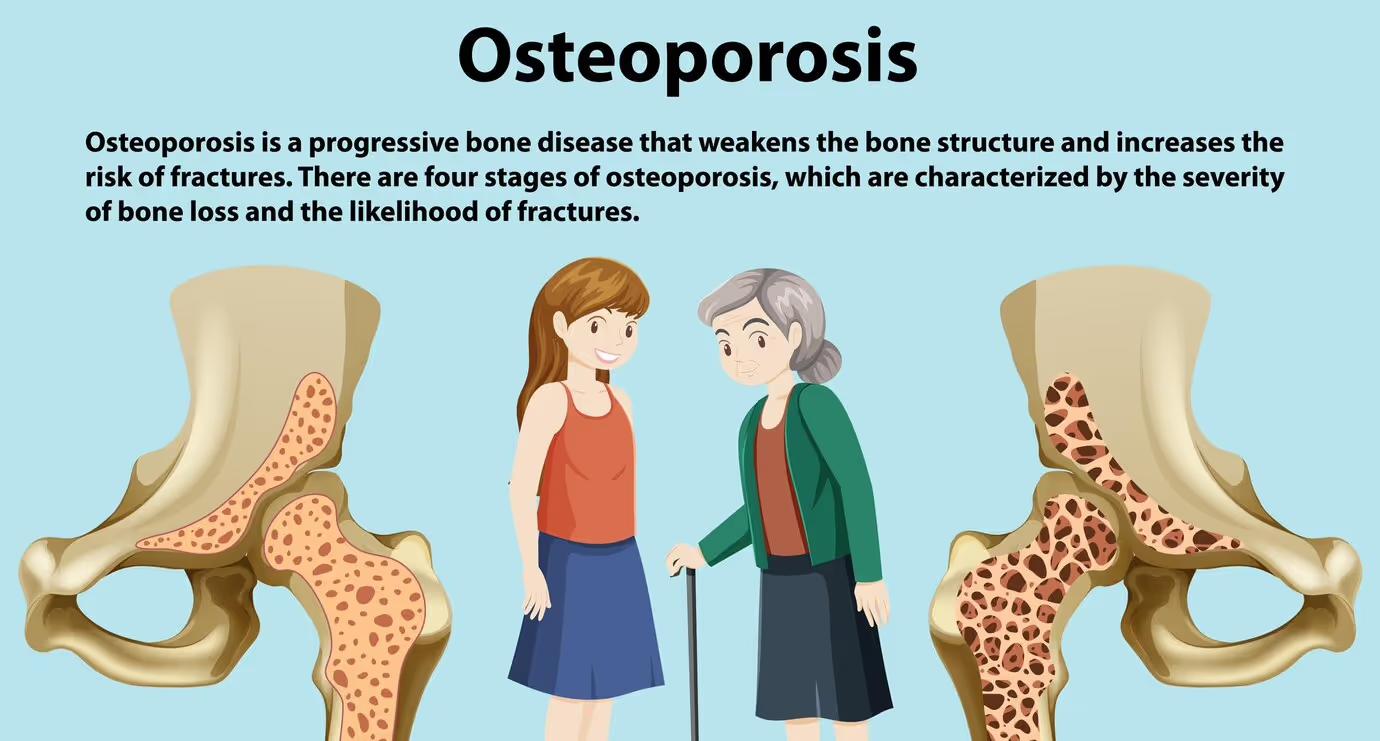
Osteoporosis is a condition that affects the bone density and quality, making the bones weak and more susceptible to fractures. In the elderly population, understanding osteoporosis is crucial for maintaining bone health and preventing fractures.
Definition of Osteoporosis
Osteoporosis is defined as a progressive bone disease characterized by low bone mineral density and deterioration of the bone tissue. This leads to increased bone fragility and a higher risk of fractures. The condition often develops silently, without any noticeable symptoms until a fracture occurs. Osteoporosis can affect any bone, but the most common sites of fractures are the hip, spine, and wrist [1].
Prevalence in the Elderly
Osteoporosis is a significant health concern in the elderly population. As people age, the risk of developing osteoporosis increases. According to studies, approximately 10 million Americans over the age of 50 have osteoporosis, and another 44 million have low bone mass, putting them at an increased risk of fractures.
The prevalence of osteoporosis in the elderly can be attributed to various factors, including age-related bone loss, hormonal changes, and lifestyle factors. Women, in particular, are at a higher risk of developing osteoporosis due to the rapid decline in estrogen levels during menopause. However, men are also susceptible to osteoporosis, albeit at a lower rate.
Understanding the definition and prevalence of osteoporosis in the elderly is essential for raising awareness about this condition and implementing preventive measures. By addressing the risk factors and adopting appropriate lifestyle modifications, individuals can reduce the impact of osteoporosis and maintain better bone health as they age.
Risk Factors for Osteoporosis
To better understand osteoporosis, it is important to be aware of the risk factors associated with this condition. Risk factors can provide valuable insights into the likelihood of developing osteoporosis. In this section, we will explore three key risk factors: age and gender, genetics and family history, and lifestyle factors.
Age and Gender
Age and gender play significant roles in the development of osteoporosis. As individuals age, their bone density tends to decrease, making them more susceptible to fractures and fractures related to osteoporosis. Women, in particular, are at a higher risk of developing osteoporosis compared to men. This is due to the hormonal changes that occur during menopause, leading to a rapid decline in bone mass. It is estimated that one in three women over the age of 50 will experience osteoporotic fractures in their lifetime. The risk for men also increases with age, though at a slower rate compared to women.
Genetics and Family History
Genetics and family history also play a role in the development of osteoporosis. If you have a parent or sibling with osteoporosis, you have a higher risk of developing the condition yourself. Certain genetic factors can affect bone density and the rate of bone loss, making some individuals more prone to osteoporosis than others [7]. It is important to be aware of your family history and discuss it with your healthcare provider, as they can provide guidance on appropriate preventive measures.
Lifestyle Factors
Lifestyle factors can significantly impact the risk of developing osteoporosis. Certain lifestyle choices can contribute to the development of weak and fragile bones. Some of the key lifestyle factors that increase the risk of osteoporosis include:
- Dietary Factors: Inadequate intake of calcium and vitamin D can compromise bone health. A diet lacking in these essential nutrients can contribute to low bone density and increase the risk of fractures.
- Physical Activity: Lack of weight-bearing exercises, such as walking, running, or strength training, can weaken bones and contribute to the development of osteoporosis. Regular exercise that puts stress on the bones helps maintain bone density and strength.
- Smoking: Smoking has been linked to reduced bone density and an increased risk of fractures. It can also interfere with the absorption of calcium, further compromising bone health.
- Alcohol Consumption: Excessive alcohol consumption can negatively affect bone health and increase the risk of fractures. It is important to consume alcohol in moderation or avoid it altogether to promote optimal bone health.
By understanding these risk factors, individuals can make informed decisions and take proactive steps to reduce their risk of developing osteoporosis. It is important to consult with a healthcare professional for personalized guidance and recommendations based on individual risk factors and overall health status.
Diagnosis and Screening Guidelines
To effectively manage osteoporosis in the elderly, it is crucial to have proper diagnosis and screening guidelines in place. This section will explore the key components of these guidelines, including bone density testing, the FRAX assessment tool, and the recommended screening frequency.
Bone Density Testing
Bone density testing, also known as dual-energy X-ray absorptiometry (DXA) or bone densitometry, is the gold standard for diagnosing osteoporosis. This non-invasive test measures the mineral content and density of bones, providing valuable information about their strength and susceptibility to fractures.
The results of a bone density test are reported as a T-score and a Z-score. The T-score compares an individual's bone density to that of a healthy young adult of the same gender, while the Z-score compares it to individuals of the same age and gender. A T-score of -2.5 or lower indicates osteoporosis, while a T-score between -1 and -2.5 indicates osteopenia, a condition of low bone density that may progress to osteoporosis.
The frequency of bone density testing depends on various factors, including age, risk factors, and previous test results. In general, the National Osteoporosis Foundation recommends that women aged 65 and older and men aged 70 and older should undergo bone density testing. Younger individuals may also be considered for testing if they have specific risk factors for osteoporosis.
FRAX Assessment Tool
The FRAX assessment tool is a valuable resource in the evaluation of fracture risk in individuals with osteoporosis. It takes into account various factors, such as age, gender, body mass index, previous fracture history, family history of hip fracture, smoking status, and alcohol consumption, to estimate the 10-year probability of a major osteoporotic fracture or hip fracture.
The FRAX assessment tool can help guide treatment decisions by identifying individuals who may benefit from pharmacological intervention. It is important to note that the FRAX tool is most applicable to postmenopausal women and men aged 50 and older.
Recommended Screening Frequency
The frequency of osteoporosis screening depends on individual risk factors and previous test results. The guidelines provided by organizations such as the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO), the International Osteoporosis Foundation (IOF), the National Osteoporosis Foundation (NOF), and the American College of Physicians (ACP) can help inform screening decisions.
In general, the following recommendations can serve as a guideline:
- Women aged 65 and older and men aged 70 and older should undergo bone density testing.
- Younger individuals should be considered for testing if they have specific risk factors for osteoporosis, such as a history of fragility fractures, prolonged use of glucocorticoid medications, or certain medical conditions.
- Those with normal bone density or osteopenia may be retested every 2-5 years, depending on individual risk factors and previous test results.
It's important to consult with a healthcare professional to determine the most appropriate screening frequency based on individual factors and guidelines.
By following the recommended diagnosis and screening guidelines, healthcare providers can identify individuals at risk for osteoporosis and initiate appropriate interventions. Early detection and treatment are essential in preventing fractures and improving the quality of life for elderly individuals at risk for osteoporosis.
Prevention Strategies
To prevent or reduce the risk of osteoporosis in the elderly, several strategies can be implemented. These include focusing on nutrition and diet, engaging in weight-bearing exercises, and implementing fall prevention measures.
Nutrition and Diet
Proper nutrition and a balanced diet are essential for maintaining bone health in the elderly. Adequate intake of calcium and vitamin D is particularly important in preventing osteoporosis. Calcium-rich foods such as dairy products, leafy greens, and fortified foods should be included in the diet to support bone density [11].
Read about: Integrating Nutrition for Total Wellness
Weight-Bearing Exercises
Engaging in weight-bearing exercises is crucial for maintaining bone health and reducing the risk of osteoporosis in the elderly. These exercises include activities that require the body to work against gravity, such as walking, jogging, dancing, and weightlifting. Regular weight-bearing exercises stimulate the bones, promoting bone formation and increasing bone density [12]. A meta-analysis has shown that walking alone has a positive effect on preserving bone mineral density in postmenopausal women [13]. It is recommended to consult with a healthcare professional or a certified fitness instructor to develop an appropriate exercise plan based on individual needs and capabilities.
Fall Prevention Measures
Falls can have severe consequences for the elderly, leading to fractures and a decline in overall well-being. Implementing fall prevention measures is crucial in reducing the risk of osteoporotic fractures. Some effective strategies include:
- Removing tripping hazards from the living environment, such as loose rugs or cluttered walkways.
- Installing handrails and grab bars in bathrooms and stairways.
- Ensuring proper lighting throughout the home.
- Wearing appropriate footwear with non-slip soles.
- Regularly reviewing medications that may affect balance or cause dizziness, in consultation with a healthcare professional.
- Engaging in exercises that improve balance and stability, such as tai chi or yoga.
- Regular eye check-ups to maintain good vision, reducing the risk of falls.
By focusing on nutrition and diet, engaging in weight-bearing exercises, and implementing fall prevention measures, it is possible to reduce the risk of osteoporosis in the elderly. It is advisable to consult with healthcare professionals or specialists who can provide personalized guidance and recommendations based on individual needs and circumstances.
Treatment Options for Osteoporosis
When it comes to treating osteoporosis in the elderly, there are several options available. The choice of treatment depends on various factors, including the severity of the condition, the individual's overall health, and any underlying medical conditions. Here, we will explore three common treatment options for osteoporosis: medications, hormone therapy, and surgical interventions.
Medications
Medications play a crucial role in the management of osteoporosis in the elderly. They are designed to slow down bone loss, increase bone density, and reduce the risk of fractures. There are several classes of medications used to treat osteoporosis, including:
- Bisphosphonates: These medications, such as alendronate and risedronate, work by inhibiting bone breakdown, thereby preserving bone mass and reducing fracture risk. They are commonly prescribed as a first-line treatment for osteoporosis.
- Selective Estrogen Receptor Modulators (SERMs): SERMs, such as raloxifene, mimic the effects of estrogen in some parts of the body, including the bones. They help to maintain bone density and reduce the risk of fractures, particularly in postmenopausal women.
- Denosumab: This medication is an injectable monoclonal antibody that targets a protein involved in bone breakdown. It helps to decrease bone loss and increase bone density.
- Teriparatide: Teriparatide is a synthetic form of parathyroid hormone that stimulates new bone growth. It is usually reserved for individuals with severe osteoporosis or those who have not responded well to other treatments.
It's important to note that the choice of medication and the duration of treatment should be determined by a healthcare professional based on the individual's specific needs and medical history. Regular monitoring and follow-up appointments are crucial to assess the effectiveness of the treatment.
Hormone Therapy
Hormone therapy, specifically estrogen therapy, may be considered for postmenopausal women with osteoporosis. Estrogen helps to maintain bone density and reduce the risk of fractures. However, hormone therapy carries certain risks and benefits and should be carefully evaluated on an individual basis.
Hormone therapy is generally recommended for women who have reached menopause and are at high risk of fractures, particularly those with significant menopausal symptoms. The decision to undergo hormone therapy should be made after considering the individual's overall health, medical history, and personal preferences. It is important to discuss the potential risks and benefits of hormone therapy with a healthcare provider.
Surgical Interventions
In certain cases, surgical interventions may be considered for the treatment of osteoporosis, particularly when fractures occur or when other treatment options have not been successful. Surgical procedures for osteoporosis include:
- Vertebroplasty and kyphoplasty: These procedures involve injecting a cement-like material into fractured vertebrae to stabilize them and relieve pain.
- Spinal fusion surgery: Spinal fusion may be recommended in cases of severe spinal deformity or instability caused by osteoporosis-related fractures.
- Joint replacement surgery: In some instances, joint replacement surgery may be necessary if osteoporosis-related fractures have severely damaged joints, such as the hip or knee.
Surgical interventions are typically considered when conservative treatment options have not provided adequate relief or when there is a significant impact on an individual's quality of life. The decision to undergo surgery should be made in collaboration with a healthcare professional and after a thorough evaluation of the risks and benefits.
It is important to note that treatment options for osteoporosis should be tailored to each individual's needs. Regular follow-up appointments with a healthcare provider are crucial to monitor the effectiveness of the chosen treatment and make any necessary adjustments. For comprehensive guidelines and recommendations, it is recommended to consult reputable sources such as the National Osteoporosis Foundation or professional medical societies.
Read about: A Comprehensive Osteoporosis Care Plan
Lifestyle Management Tips
In addition to medical interventions, lifestyle management plays a crucial role in managing osteoporosis in the elderly. By making certain lifestyle changes, individuals can improve their bone health and reduce the risk of fractures. Here are some key lifestyle management tips to consider:
Smoking Cessation
Smoking has been shown to have detrimental effects on bone health. It increases the risk of osteoporosis and fractures by interfering with the body's ability to absorb calcium and impairs bone formation. Quitting smoking is essential for maintaining healthy bones.
According to the Centers for Disease Control and Prevention, smoking affects nearly every organ in the body and is a major cause of preventable diseases. By quitting smoking, individuals can improve their overall health and reduce the risk of developing osteoporosis.
Alcohol Consumption
Excessive alcohol consumption can negatively impact bone health. Long-term and heavy alcohol use can lead to decreased bone formation, increased bone loss, and an increased risk of fractures. It's important for individuals with osteoporosis to limit their alcohol intake.
The National Institute on Alcohol Abuse and Alcoholism highlights the effects of alcohol on the body, including bone health [16]. Moderate alcohol consumption, defined as up to one drink per day for women and up to two drinks per day for men, may not have significant negative effects. However, excessive alcohol consumption should be avoided.
Read about: Expert Home Healthcare Services
Regular Medical Check-ups
Regular medical check-ups are important for monitoring bone health and managing osteoporosis. These check-ups allow healthcare professionals to assess the effectiveness of treatment plans, evaluate bone density, and make any necessary adjustments.
By staying up-to-date with regular check-ups, individuals can receive timely interventions and make informed decisions about their bone health. Regular check-ups also provide an opportunity for healthcare providers to discuss lifestyle modifications and offer guidance specific to each individual's needs.
The American Heart Association emphasizes the importance of regular check-ups for overall health maintenance. Mayo Clinic also suggests that regular check-ups help detect potential health issues early, allowing for prompt intervention and improved outcomes [18].
By incorporating these lifestyle management tips into daily routines, individuals can take proactive steps to manage osteoporosis and maintain optimal bone health. It's important to remember that these tips should be implemented alongside medical recommendations and personalized advice from healthcare professionals.
References
- https://www.bones.nih.gov/health-info/bone/osteoporosis/overview
- https://www.bones.nih.gov/health-info/bone/osteoporosis/what-women-need-to-know
- https://www.osteoporosis.foundation/facts-statistics
- https://www.niams.nih.gov/health-topics/bone-health
- https://www.osteoporosis.foundation/lifestyle-factors
- https://www.mayoclinic.org/diseases-conditions/osteoporosis/symptoms-causes/syc-20351968
- https://www.niaaa.nih.gov/alcohols-effects-health/alcohols-effects-body
- https://www.heart.org/en/health-topics/consumer-healthcare/why-get-regular-check-ups
- https://www.mayoclinic.org/healthy-lifestyle/adult-health/in-depth/health-checkups/art-20044944
































































































